Abstract
Purpose
SeptiFast is a real-time PCR assay which targets ribosomal DNA sequences of bacteria and fungi, enabling detection and identification of the commonest pathogens in blood within a few hours, including those acquired in healthcare settings. We report here the first detailed assessment of SeptiFast that focuses on healthcare-associated bloodstream infections which develop during routine critical care.
Methods
This was a prospective multicentre study designed to compare the clinical diagnostic accuracy of SeptiFast versus microbiological culture and independent clinical adjudication. This Phase III diagnostic study was performed in an adequately sized cohort of adult patients who developed new signs of suspected bloodstream infection while receiving routine critical care.
Results
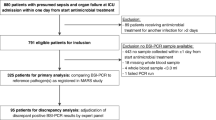
Of 1,006 new episodes of suspected bloodstream infection in 853 patients, 922 (92 %) of these episodes in 795 patients met the inclusion criteria of the study. Patients had been exposed to a median of 8 days (interquartile range 4–16) of hospital care and had received high levels of organ support and recent antibiotic exposure. The SeptiFast test, when compared with bloodstream infection at the species/genus level, had a greater specificity [0.86, 95 % confidence interval (CI) 0.83–0.88] than sensitivity (0.50, 95 % CI 0.39–0.61). There was a low prevalence of blood culture-proven pathogens (9.2 %, 95 % CI 7.4–11.2 %), and the post-test probabilities of both a positive (26.3 %, 95 % CI 19.8–33.7 %) and a negative SeptiFast test (5.6 %, 95 % CI 4.1–7.4 %) indicated potential limitations of this technology in diagnosing bloodstream infection.
Conclusion
When compared with blood culture, SeptiFast is likely to have limited utility for the diagnosis of healthcare-associated bloodstream infection in critical care patients despite its potential to deliver results more rapidly.
Similar content being viewed by others
References
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302:2323–2329
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Keohane C, Denham CR, Bates DW (2013) Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 173:2039–2046
Comptroller and Auditor General (2009) Reducing healthcare associated infection in hospitals in England. National Audit Office HC 560, London
European Centre for Disease Prevention and Control (2013) Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals. European Centre for Disease Prevention and Control, Stockholm
Health Protection Agency (2005) Investigation of blood cultures (for organisms other than mycobacterium species). Standards Unit BSOP 37, London
Davies SC (2013) Annual report of the chief medical officer, vol. 2, 2011. Infections and the rise of antimicrobial resistance. Department of Health, London
Dark PM, Dean P, Warhurst G (2009) Bench-to-bedside review: the promise of rapid infection diagnosis during sepsis using polymerase chain reaction-based pathogen detection. Crit Care 13:217–222
World Health Organisation (2012) The evolving threat of antimicrobial resistance: options for action. World Health Organisation, Geneva
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Beale RJ, Webb, Vincent JL, Moreno R (2012) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 39:165–228
Lisenfeld O, Lehmann L, Hunfeld K-P, Kost G (2014) Molecular diagnosis of sepsis: new aspects and recent developments. Eur J Microbiol Immunol 4:1–25
Skvarc M, Stubljar D, Rogina P, Kaasch AJ (2013) Non culture-based methods to diagnose bloodstream infection: does it work? Eur J Microbiol Immunol 3:97–104
Lehmann LE, Hunfeld KP, Emrich T, Haberhausen G, Wissing H, Hoeft A, Stüber F (2008) A multiplex real-time PCR assay for rapid detection and differentiation of 25 bacterial and fungal pathogens from whole blood samples. Med Microbiol Immunol 197:313–324
Chang SS, Hsieh WH, Liu TS, Lee SH, Wang CH, Chou HC, Yeo YH, Tseng CP, Lee CC (2013) Multiplex PCR system for rapid detection of pathogens in patients with presumed sepsis—a systemic review and meta-analysis. PLoS One 8:e62323
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC (2003) Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ 326:341–344
National Institute for Health Research. Available at:http://www.nets.nihr.ac.uk/projects/hta/081316
Dark P, Dunn G, Chadwick P, Young D, Bentley A, Carlson G, Warhurst G (2011) The clinical diagnostic accuracy of rapid detection of healthcare-associated bloodstream infection in intensive care using multi-pathogen real-time polymerase chain reaction (real-time PCR) technology. BMJ Open 1:e000181
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis definitions Conference. Intensive Care Med 29:530–538
Hospital Infection Society (2007) The third prevalence survey of healthcare associated infections in acute hospitals in England 2006: report for Department of Health (England). Department of Health, London
Buderer NM (1996) Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med 3:895–900
http://www.ukas.com/services/CPA/Clinical_Pathology_Accreditation_CPA.asp
Felton TW, Sander R, Al-Aloul M, Dark P, Bentley AM (2009) Can a score derived from the critical care minimum data set be used as a marker of organ dysfunction?—a pilot study. BMC Res Notes 2:77
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–474
Westh H, Lisby G, Breysse F, Böddinghaus B, Chomarat M, Gant V, Goglio A, Raglio A, Schuster H, Stuber F, Hoeft A, Wissing (2009) Multiplex real-time PCR and blood culture for identification of bloodstream pathogens in patients with suspected sepsis. Clin Microbiol Infect 15:544–551
Yanagihara K, Kitagawa Y, Tomonaga M, Tsukasaki K, Kohno S, Seki M, Sugimoto H, Shimazu T, Tasaki O, Matsushima A, Ikeda Y, Okamoto S, Aikawa N, Hori S, Obara H, Ishizaka A, Hasegawa N, Takeda J, Kamihira S, Sugahara K, Asari S, Murata M, Kobayashi Y, Ginba H, Sumiyama Y, Kitajima M (2010) Evaluation of pathogen detection from clinical samples by real-time polymerase chain reaction using a sepsis pathogen DNA detection kit. Crit Care 14:R159
Lucignano B, Ranno S, Liesenfeld O, Pizzorno B, Putignani L, Bernaschi P, Menichella D (2011) Multiplex PCR allows rapid and accurate diagnosis of bloodstream infections in newborns and children with suspected sepsis. J Clin Microbiol 49:2252–2258
Louie RF, Tang Z, Albertson TE, Cohen S, Tran NK, Kost GJ (2008) Multiplex polymerase chain reaction detection enhancement of bacteremia and fungemia. Crit Care Med 36:1487–1492
Mermel LA, Maki DG (1993) Detection of bacteremia in adults: consequences of culturing an inadequate volume of blood. Ann Intern Med 119:270–272
Arpi M, Bentzon MW, Jensen J, Frederiksen W (1989) Importance of blood volume cultured inthe detection of bacteremia. Eur J Clin Microbiol Infect Dis 8:838–842
Pletz MW, Wellinghausen N, Welte T (2011) Will polymerase chain reaction (PCR) based diagnostics improve outcome in septic patients? A clinical view. Intensive Care Med 37:1069–1076
Hettwer S, Wilhelm J, Schurmann M, Ebelt H, Hammer D, Amoury M, Hofmann F, Oehme A, Wilhelms D, Kekule AS, Kloss T, Werdan K (2011) Microbial diagnostics in patients with presumed severe infection in the emergency department. Intensivmed Notfallmed 107:53–62
Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM (2007) Evaluation of diagnostic tests when there is no gold standard. A review of methods. Health Technol Assess 11(50):iii, ix-51
Huttunen R, Syrjänen J, Vuento R, Aittoniemi J (2013) Current concepts in the diagnosis of blood stream infections. Are novel molecular methods useful in clinical practice? Int J Infect Dis 17:934–938
Acknowledgements
We would like to thank Sister Tracey Evans for coordinating patient recruitment with Sisters Alison Royle, Alison Middleton and Elaine Coghlan. We also thank Dr. Gareth Thomas, Dr. John Hopper, Dr. Jane Eddleston, Dr. Paul Dean and all of the critical care and laboratory staff at the recruitment sites: Salford Royal NHS Foundation Trust, University Hospital of South Manchester NHS Foundation Trust, Central Manchester University Hospitals NHS Foundation Trust and East Lancashire Hospitals NHS Trust. We appreciate the molecular assay laboratory support from Pamela Davies and administration assistance from various NIHR Clinical Trial Graduate Interns during study planning and conduct: Matthew Langley, Claire Wilson, Daniel Graham and Kate Timms. We thank Dr. Neil Pendleton, Professor John Wain and Mrs Rosemary Martin for their independent leadership and contributions to the NIHR HTA Trial Steerign Committee. We would like to thank Professor Bill Ollier, Rachel Georgiou and their staff in the Research and Development Department at Salford Royal NHS Foundation Trust (the study Sponsors) for their support and advice throughout the study. The study was funded by the UK Health Technology Assessment (HTA) programme of the National Institute of Health Research: grant number NIHR HTA 08/13/16.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take home message
We report a phase III diagnostic accuracy study of SeptiFast real-time PCR in the setting of healthcare associated infection in critical care. Our main finding was that when compared with blood culture, SeptiFast is likely to have limited utility for the diagnosis of bloodstream infection despite its potential to deliver results more rapidly.
Study registration: UK Health Technology Assessment programme of the National Institute of Health Research (08/13/16).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Warhurst, G., Maddi, S., Dunn, G. et al. Diagnostic accuracy of SeptiFast multi-pathogen real-time PCR in the setting of suspected healthcare-associated bloodstream infection. Intensive Care Med 41, 86–93 (2015). https://doi.org/10.1007/s00134-014-3551-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3551-x