Abstract
Background:
Colonoscopic surveillance provides the best practical means for preventing colorectal cancer (CRC) in inflammatory bowel disease (IBD) patients. Strong evidence for improved survival from surveillance programmes is sparse.
Method:
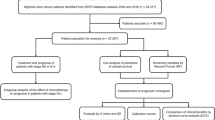
The aim of this study was to compare tumour stage and survival of IBD patients with CRC who were a part of a surveillance programme with those who were not. A nationwide pathology database (PALGA (pathologisch anatomisch landelijk geautomatiseerd archief)) was consulted to identify IBD patients with CRC treated in all eight university hospitals in The Netherlands over a period of 15 years. Patients were assigned to the surveillance group when they had undergone one or more surveillance colonoscopies before a diagnosis of CRC. Patients who had not undergone surveillance served as controls. Tumour stage and survival were compared between the two groups.
Results:
A total of 149 patients with IBD-associated CRC were identified. Twenty-three had had colonoscopic surveillance before CRC was discovered. The 5-year CRC-related survival rate of patients in the surveillance group was 100% compared with 74% in the non-surveillance group (P=0.042). In the surveillance group, only one patient died as a consequence of CRC compared with 29 patients in the control group (P=0.047). In addition, more early tumour stages were found in the surveillance group (P=0.004).
Conclusions:
These results provide evidence for improved survival from colonoscopic surveillance in IBD patients by detecting CRC at a more favourable tumour stage.
Similar content being viewed by others
Main
The increased risk of colorectal cancer (CRC) in patients with inflammatory bowel disease (IBD) has been well documented (Eaden et al, 2001; Jess et al, 2005). In an effort to detect dysplasia or early stage cancer, it is advised that patients should enter a surveillance programme according to the guidelines of the American Gastroenterological Association (Winawer et al, 2003) or of the British Society of Gastroenterology (Eaden and Mayberry, 2002). Although not flawless, it is currently the best tool available to detect early-stage neoplasia or prevent CRC in patients with IBD. The level of evidence for its effectiveness, however, is low and has only been studied in patients with ulcerative colitis (Collins et al, 2006). The ideal setup to evaluate the effectiveness of surveillance programmes would be a randomised trial with CRC-related mortality as the primary end point. Unfortunately, such a trial does not exist and probably never will be performed because of practical and ethical considerations (Bernstein, 1998). Therefore, retrospective studies are probably the best alternative to assess the effectiveness of colonoscopic surveillance.
A recent review by the Cochrane Collaboration (Collins et al, 2006) identified three studies that presented indirect evidence for improved survival from colonoscopic surveillance in ulcerative colitis patients (Lashner et al, 1990; Choi et al, 1993; Karlen et al, 1998). These studies either had a low number of patients with IBD-associated CRC or a low number of patients in a surveillance programme, which prevented the outcomes from reaching statistical significance.
We recently reported on time intervals between the diagnosis of IBD and CRC in a large cohort of patients with IBD-associated CRC, collected from all university medical centres in The Netherlands using a nationwide pathology database (Lutgens et al, 2008). The aim of this retrospective study was to compare tumour stage and survival in this cohort between patients who were a part of a surveillance programme with those who were not.
Materials and methods
Search strategy
Pathologisch anatomisch landelijk geautomatiseerd archief (PALGA), the nationwide network and registry of histo- and cytopathology (Casparie et al, 2007), contains pathology reports generated in the Netherlands dating back to 1971. These reports are concluded with diagnostic terms in line with SNOMED (systematised nomenclature of medicine) terminology and were used to search for patients with IBD-associated CRC. PALGA achieved nationwide coverage in 1990. For that reason, a search for the time period between January 1990 and July 2006 in all eight Dutch university medical centres for synchronous or metachronous diagnoses of IBD and CRC was conducted. The following combinations of search terms were used: ulcerative colitis and adenocarcinoma; Crohn's disease and adenocarcinoma; colon and colitis and adenocarcinoma; colon and inflammation and adenocarcinoma; colon and chronic inflammation and adenocarcinoma; colon and idiopathic colitis and adenocarcinoma; colon and adenocarcinoma and active inflammation. Only patients with a confirmed histological diagnosis of inflammatory bowel disease and CRC were included.
The PALGA search engine ensures patient privacy by supplying anonymous data. Only the patient's own physician was able to link PALGA identification codes to real patient identification codes. The treating physician in each university medical centre subsequently supplied only the first author with anonymous data. No personal patient data were recorded.
Data extraction
The following data were collected from patient charts by one investigator (ML): type of IBD, gender, age at IBD diagnosis, age at CRC diagnosis, date of onset of symptoms, date of IBD diagnosis, date of CRC diagnosis, date of start of surveillance, intervals between surveillance colonoscopies, date of end of follow-up, cause of death, tumour stage in the resection specimen or by radiological imaging if the patient was not operated, concurrent primary sclerosing cholangitis, existing co-morbidity, history of smoking and alcohol use, and history of 5-amino-salycilic acid (5-ASA) medication. A diagnosis of primary sclerosing cholangitis had to be made with retrograde cholangiopancreatography, magnetic resonance cholangiopancreatography, or liver biopsy. Co-morbidity was defined as severe cardiac, severe pulmonary, severe renal, severe liver dysfunction, or malignancy other than CRC.
Surveillance criterion
A patient was assigned to the surveillance group when before CRC diagnosis at least one or more surveillance colonoscopies at regular intervals (every 1–3 years) had been performed. The remainder of the patients were assigned to the non-surveillance group and served as controls. The surveillance quality had to meet the standard that is described by current guidelines (Eaden and Mayberry, 2002; Winawer et al, 2003). This entails the intent to detect neoplasia by taking four random biopsies every 10 cm of the colon in addition to targeted biopsies of suspicious areas during that colonoscopy. No attempt was made to compare surveillance colonoscopies with each other on the basis of frequency or number of biopsies.
Patients who were under regular surveillance for multiple years, but for some reason had skipped one colonoscopy, were only assigned to the surveillance group if the longest lapse since the last colonoscopy was 3 years or less. To minimise selection bias, patients in whom the diagnosis of CRC was made by colonoscopy according to surveillance protocol for the first time (thus not yet enrolled in a surveillance programme) were not assigned to the surveillance group when the reason for this first surveillance colonoscopy was new or recurrent symptoms of disease.
Statistical analysis
The χ2 test, Fisher's exact test, and Student's t–test were used where appropriate to compare patient characteristics between the two groups. Kaplan–Meier (Kaplan and Meier, 1958) and Cox regression analyses were used for survival calculations. The primary study end points were CRC related or overall death. The end of follow-up was either the end of study date (1 July 2006) or date of death. When a patient was lost to follow-up, the date of the last visit to the hospital was recorded as end of follow-up. The Tarone–Ware test of equality of survival distributions was used to compare differences between survival curves. Tumour stages were grouped according to the sixth edition staging system of the American Joint Committee on Cancer (Greene et al, 2002; Sobin and Wittekind, 2002). The χ2 test and Fisher's exact test were used where it was appropriate to compare tumour stages between the surveillance and non-surveillance groups. P-values <0.05 were considered to be statistically significant. SPSS software for windows version 14.0, SPSS Inc, was used for all statistical analyses.
Results
Our search identified 166 patients, of whom 17 were excluded. The reasons for exclusion were: no histological confirmed diagnosis of IBD (n=11), suspected adenocarcinoma in the biopsy sample that could not be reproduced in the colectomy specimen (n=2), a focus of micro-carcinoid instead of adenocarcinoma (n=2), unknown date of IBD diagnosis (n=1), and occurrence of CRC before IBD was diagnosed (n=1). This left 149 cases for analysis. Twenty-three patients had undergone one or more surveillance colonoscopies before the diagnosis of CRC and were analysed as the surveillance group. Surveillance was started after a median of 14.3 (std 8.0) years after histological diagnosis of IBD. CRC developed after a median of 6.4 years (range 1–21) after initiation of surveillance. The remaining 126 patients were assigned to the non-surveillance control group. Patient characteristics are shown in Table 1. No statistically significant differences were found between the two groups for any of the variables.
Follow-up after a diagnosis of CRC was complete for 114 (79%) patients until the study end date or death. Thirty-one (21%) patients were lost to follow-up. Four of these 31 patients, two in the surveillance group and two in the non-surveillance group, were lost to follow-up immediately after diagnosis of CRC and were therefore excluded from the survival analyses.
Overall, 42 of 145 (29%) patients died. The cause of death was directly related to metastasised CRC in 30 patients. Of the remaining, six patients died from metastasis of a different primary tumour (cholangiocarcinoma (n=3), renal cell tumour (n=1), urothelial carcinoma (n=1), primary tumour of the stomach (n=1)), and another six patients died after complications related to colectomy. In the surveillance group, only one patient died because of CRC compared with 29 patients in the non-surveillance control group (P=0.047). The overall 5-year survival rates in the surveillance group and in the non-surveillance control group were 100% and 65%, respectively (P=0.029) (Figure 1). CRC-related 5-year mortalities were 0% and 26% in the surveillance and non-surveillance groups, respectively (P=0.042) (Figure 1). In addition, a multivariate Cox regression analysis, including type of IBD, concurrent primary sclerosing cholangitis, age at CRC diagnosis, and co-morbidity as co-variables confirmed the association between colonoscopic surveillance and improved survival with reduced CRC-related mortality; however, this did not reach statistical significance (P=0.10) (Table 2).
Survival analysis for CRC-related and overall mortality. The Tarone–Ware test of equality of survival distribution was used to compare survival between the two groups. CRC-related mortality is presented by solid squares and line. Overall mortality is presented by outlined squares and line. For CRC-related mortality, the 5-year survival in the surveillance group (solid squares) was 100% compared with 74% in the non-surveillance group (solid black line) (P=0.029); the primary end point was date of death due to CRC; cases were censored for date of end of study, date of death related to any other primary malignancy, date of death related to colectomy, date of death by any other cause, and date of lost to follow-up. For overall mortality, the 5-year survival in the surveillance group (outlined squares) was 100% compared with 65% in the non-surveillance group (outlined line; P=0.042); the primary end point was date of death; cases were censored for date of end of study period and date of lost to follow-up. CRC, colorectal cancer.
Eleven patients in the non-surveillance group were diagnosed with IBD and CRC simultaneously. Exclusion from analysis of these patients strengthens the effect. The 5-year overall mortality is 0% in the surveillance group and 36% in the non-surveillance group (P=0.02). For CRC-related mortality, these percentages are 0% and 29% (P=0.03). This effect also remains visible in the multivariate analysis, although again it is not statistically significant (Table 2).
In 10 out of 149 patients (7%), we did not have information regarding 5-ASA prescription. This leaves 139 patients for analysis, of whom 119 (86%) have used a 5-ASA preparation during the course of their disease. Of these 119 patients, 64 (54%) used 5-ASA medication for more than three-quarters of their disease duration. Nevertheless, all these patients developed CRC despite the chemopreventive nature of 5-ASAs. As mentioned earlier, 4 out of 149 patients were excluded when evaluating survival because they were lost to follow-up directly after CRC diagnosis. Therefore, 135 patients remain for 5-ASA analysis between groups. Twenty patients were in the surveillance group and 115 in the non-surveillance group. All 20 patients (100%) in the surveillance group had used 5-ASA preparations during their disease. In the non-surveillance group, 96 out of 115 (77%) had used 5-ASA preparations. This difference showed a trend but was not statistically significant (P=0.08). Furthermore, when included in the multivariate cox regression analysis, it has no influence on survival (P=0.96), whereas the effect of surveillance (P=0.098) remains unchanged.
Tumour stages of the two groups are separately shown in Table 3. Tumours were staged by a pathologist on the resection specimen in 138 patients (93%) according to the TNM classification. Information on TNM stage could not be retrieved in 11 patients (7%) for the following reasons: either the patients were not operated on because of metastatic disease (n=6), or a fully detailed pathology report of resection specimen was not retrievable (n=5). In patients from the surveillance group, the observed number of lower-stage tumours was higher than the expected number. This effect was statistically significant when Stage 0 and 1 tumours were compared with all higher stages between the two groups. In the surveillance group, 12 patients (52%) had Stage 0 and 1 tumours compared with 28 patients (24%) in the non-surveillance group (P=0.004). Moreover, the same effect was also observed in the opposite direction with a statistically significantly lower number of patients with Stages 3B-C and 4 tumours: four patients (17%) in the surveillance group compared with 48 patients (42%) in the non-surveillance group (P=0.049).
Despite surveillance, four cancers in the surveillance group were diagnosed as a consequence of new or altered symptoms of disease. These so-called interval cancers had varying tumour stages: T1N0M0, T2N1M0, T3N0M0, and T4N0M0. The interval since last surveillance colonoscopy was 10, 14, 8, and 7 months, respectively, and the patients were on 1-, 2-, 1, and 3-yearly intervals of surveillance colonoscopies.
Discussion
This series shows an improved survival in IBD patients who developed CRC and in whom colonoscopic surveillance was performed. It provides evidence showing the efficacy of surveillance on CRC-related mortality with sufficient numbers of patients with IBD-associated CRC. CRC-related mortality was significantly lower in the surveillance group, with a 5-year survival rate of 100% in the surveillance group and 74% in the non-surveillance group. This effect can be explained by the detection of earlier-stage CRC in the surveillance group, which translates into a better prognosis.
This report adds to the relatively small body of evidence, indicating survival benefit through a surveillance strategy in ulcerative colitis. We feel that it is prudent to join the ulcerative colitis and Crohn's colitis data, because there is increasing evidence that the pathogenesis and natural behaviour of inflammation-associated dysplasia in ulcerative colitis and Crohn's disease do not differ, and the risk of CRC is increased in both (1,2). A recent systematic review (Collins et al, 2006) by the Cochrane collaboration detected only three papers (Lashner et al, 1990; Choi et al, 1993; Karlen et al, 1998) that properly addressed the question of surveillance effectiveness for patients with ulcerative colitis. Other surveillance studies lacked valid control groups (Rosenstock et al, 1985; Lofberg et al, 1990; Nugent et al, 1991; Jonsson et al, 1994; Friedman et al, 2001; Biasco et al, 2002; Hata et al, 2003) or were not designed to answer this question (Eaden et al, 2000). The reviewers of the Cochrane paper concluded that all three publications pointed towards a beneficial effect of surveillance on survival, but that the evidence was indirect. Lashner et al (1990) showed an improved overall survival in the surveillance group, but were unable to show that this was secondary to a reduced CRC-related mortality. Similarly, they could not find a difference in tumour stage between the two groups. Choi et al (1993) published a small series of 41 patients who developed CRC associated with ulcerative colitis, of whom 19 were in a colonoscopic surveillance programme and 22 were not. In their series, as in ours, CRC was detected at a significantly earlier stage in patients who had undergone colonoscopic surveillance. Karlen et al, (1998) identified a trend towards a protective effect of colonoscopic surveillance.
The strength of the current series lies in the high number of cases with IBD-associated CRC available for analysis and the strict criteria for inclusion in the surveillance group. Moreover, no differences between the two groups in age at cancer diagnosis, length of follow-up, and interval between onset of IBD and CRC diagnosis were found, eliminating confounding from differences in these variables (Table 1). The multivariate analysis confirmed the association between colonocopic surveillance and improved survival, but failed to reach statistical significance most probably because of a type II error resulting from multiple variables in the analysis (Table 2). The putative additional effect of smoking or alcohol could not be evaluated in this analysis because of high percentages of missing values.
Selection is a potential bias that needs consideration. Patients who presented with diarrhoea or rectal bleeding and were subsequently diagnosed with both IBD and CRC could very well have affected the observed results. These patients would not have participated in an endoscopic surveillance programme and were probably only detected with IBD because of their CRC-related symptoms. Eleven patients in our series were simultaneously diagnosed with IBD and CRC. However, our results for CRC-related tumour stage and mortality between groups did not change when patients whose interval between diagnosis of IBD and CRC was less than 1 year were excluded from the analysis. This is not surprising as these patients were probably not different from the patient group that did not undergo surveillance. It seems likely that these individuals did not seek medical care for their condition because of the absence of symptoms, and presented some years after the start of the disease because of symptoms that were found to be (at least partly) CRC related.
It is well recognised that 5-ASA is thought to be chemopreventive for neoplasia. We collected data on medication use in all patients. However, the retrospective design of our data collection warrants us to be careful with its interpretation. Not all physicians meticulously registered the exact duration of medication usage, nor did we have insight into medication adherence.
Lead-time bias is known to influence screening and surveillance data (Kramer, 2004). However, lead-time bias only occurs if the intervention (in this case earlier tumour detection) does not affect the terminal event (in this case mortality by CRC). In the case of CRC, lead-time bias is probably not a significant problem, as earlier diagnosis of CRC at a more favourable stage does improve survival in a beneficial manner (Ries et al, 2007; Levin et al, 2008). Others have questioned the importance of lead-time bias in CRC-screening studies as well (Ransohoff and Lang, 1991).
Because of the lack of randomisation, volunteer bias might have influenced results. The patients in the surveillance group could have been more health conscious, leading to an earlier diagnosis of CRC. In our study, however, the mean duration of disease until CRC detection was longer in the surveillance group (22.7 vs 19.3 years). Therefore, it is not very likely that volunteer bias had a major role in this study.
Four cancers in the surveillance group were found to be interval cancers. This has been observed by others as well (Choi et al, 1993). We did not extract information on the exact number of biopsies for each surveillance colonoscopy separately and therefore cannot comment upon whether these interval cancers may be attributable to sub-optimal practice during the previous surveillance colonoscopy. The occurrence of altered bowel symptoms may lead to a diagnosis of CRC. Whether interval cancers are due to a failure of detection during previous colonoscopy or to a rapid progression of cancer is difficult to determine. Back-to-back colonoscopy in patients without IBD has shown that the miss rate for adenomas is 6–27%, which, among others, depends on adenoma size (Rex et al, 1997). In addition, in all four of these patients, unifocal low-grade dysplasia (LGD) had been diagnosed before the diagnosis of CRC in a part of the colon close to the location at which subsequently CRC was detected. Therefore, either the CRC was missed at the previous colonoscopy or LGD had progressed towards CRC between the two colonoscopies. Most clinicians recommend colectomy for high-grade dysplasia; however, management for LGD is controversial. Only 5% of Dutch gastroenterologists recommend colectomy for unifocal LGD. A little under 30% of Dutch gastroenterologists recommend colectomy in the case of multi-focal LGD (van Rijn et al, 2009).
Finally, referral centre bias deserves attention. All included cases in this study were primarily treated in or referred to tertiary university medical centres, which may have led to the introduction of bias towards patients with more severe disease. Regarding the level of risk of CRC in IBD patients, this kind of bias might be of major importance, but it is less clear how this may affect the main outcome of this study as index and control patients all originate from referral hospitals. Although it is true that the results from this study cannot be translated to the general IBD population unequivocally, to date, no study exists comparing survival outcome between IBD patients from referral centres and population-based cohorts undergoing surveillance.
In conclusion, the patients in the surveillance group showed statistically significant lower CRC-related mortality and more favourable tumour stages. The evidence for improved survival in this paper strengthens the notion that colonoscopic surveillance in patients with longstanding IBD is beneficial and should be performed in patients with a presumed high-risk profile.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bernstein CN (1998) Challenges in designing a randomized trial of surveillance colonoscopy in IBD. Inflamm Bowel Dis 4: 132–141
Biasco G, Rossini FP, Hakim R, Brandi G, Di BM, Di FG, Calabrese C, Santucci R, Miglioli M (2002) Cancer surveillance in ulcerative colitis: critical analysis of long-term prospective programme. Dig Liver Dis 34: 339–342
Casparie M, Tiebosch ATMG, Burger G, Blaauwgeers H, Pol Avan de de Bruïne AP, Meijer GA (2007) Pathology databanking and biobanking in The Netherlands, a central role for PALGA, the nationwide histopathology and cytopathology data network and archive. Cell Oncol 29: 19–24
Choi PM, Nugent FW, Schoetz Jr DJ, Silverman ML, Haggitt RC (1993) Colonoscopic surveillance reduces mortality from colorectal cancer in ulcerative colitis. Gastroenterology 105: 418–424
Collins PD, Mpofu C, Watson AJ, Rhodes JM (2006) Strategies for detecting colon cancer and/or dysplasia in patients with inflammatory bowel disease. Cochrane Database Syst Rev 19 (2): CD000279
Eaden J, Abrams K, Ekbom A, Jackson E, Mayberry J (2000) Colorectal cancer prevention in ulcerative colitis: a case–control study. Aliment Pharmacol Ther 14: 145–153
Eaden JA, Abrams KR, Mayberry JF (2001) The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut 48: 526–535
Eaden JA, Mayberry JF (2002) Guidelines for screening and surveillance of asymptomatic colorectal cancer in patients with inflammatory bowel disease. Gut 51 (Suppl 5): V10–V12
Friedman S, Rubin PH, Bodian C, Goldstein E, Harpaz N, Present DH (2001) Screening and surveillance colonoscopy in chronic Crohn′s colitis. Gastroenterology 120: 820–826
Greene FL, Page DL, Fleming ID (2002) AJCC cancer staging manual 6th ed Springer: New York, Ref Type: Report
Hata K, Watanabe T, Kazama S, Suzuki K, Shinozaki M, Yokoyama T, Matsuda K, Muto T, Nagawa H (2003) Earlier surveillance colonoscopy programme improves survival in patients with ulcerative colitis associated colorectal cancer: results of a 23-year surveillance programme in the Japanese population. Br J Cancer 89: 1232–1236
Jess T, Gamborg M, Matzen P, Munkholm P, Sorensen TI (2005) Increased risk of intestinal cancer in Crohn's disease: a meta-analysis of population-based cohort studies. Am J Gastroenterol 100: 2724–2729
Jonsson B, Ahsgren L, Andersson LO, Stenling R, Rutegard J (1994) Colorectal cancer surveillance in patients with ulcerative colitis. Br J Surg 81: 689–691
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53: 457–481
Karlen P, Kornfeld D, Brostrom O, Lofberg R, Persson PG, Ekbom A (1998) Is colonoscopic surveillance reducing colorectal cancer mortality in ulcerative colitis? A population-based case–control study. Gut 42: 711–714
Kramer BS (2004) The science of early detection. Urol Oncol 22 (4): 344–347
Lashner BA, Kane SV, Hanauer SB (1990) Colon cancer surveillance in chronic ulcerative colitis: historical cohort study. Am J Gastroenterol 85: 1083–1087
Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Dash C, Giardiello FM, Glick S, Johnson D, Johnson CD, Levin TR, Pickhardt PJ, Rex DK, Smith RA, Thorson A, Winawer SJ (2008) Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 134: 1570–1595
Lofberg R, Brostrom O, Karlen P, Tribukait B, Ost A (1990) Colonoscopic surveillance in long-standing total ulcerative colitis – a 15-year follow-up study. Gastroenterology 99: 1021–1031
Lutgens MWMD, Vleggaar FP, Schipper MEI, Stokkers PC, van der Woude CJ, Hommes DW, de Jong DJ, Dijkstra G, van Bodegraven AA, Oldenburg B, Samsom M (2008) High frequency of early colorectal cancer in inflammatory bowel disease. Gut 57: 1246–1251
Nugent FW, Haggitt RC, Gilpin PA (1991) Cancer surveillance in ulcerative colitis. Gastroenterology 100: 1241–1248
Ransohoff DF, Lang CA (1991) Screening for colorectal cancer. N Engl J Med 325: 37–41
Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA, Mark DG (1997) Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 112: 24–28
Ries L, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK (2007) SEER Cancer Statistics Review, 1975–2004. National Cancer Institute: Bethesda MD
van Rijn AF, Fockens P, Siersema PD, Oldenburg B (2009) Adherence to surveillance guidelines for dysplasia and colorectal carcinoma in ulcerative and Crohn's colitis patients in the Netherlands. World J Gastroenterol 15: 226–230
Rosenstock E, Farmer RG, Petras R, Sivak Jr MV, Rankin GB, Sullivan BH (1985) Surveillance for colonic carcinoma in ulcerative colitis. Gastroenterology 89: 1342–1346
Sobin LH, Wittekind CH (2002) TNM classification of malignant tumors' 6th ed Wiley-Liss: New York, Ref Type: Report
Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, Ganiats T, Levin T, Woolf S, Johnson D, Kirk L, Litin S, Simmang C (2003) Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology 124: 544–560
Acknowledgements
The authors thank Ms Mariël Caspari, MD, from the Prismant Insitute for her help with our initial PALGA search.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lutgens, M., Oldenburg, B., Siersema, P. et al. Colonoscopic surveillance improves survival after colorectal cancer diagnosis in inflammatory bowel disease. Br J Cancer 101, 1671–1675 (2009). https://doi.org/10.1038/sj.bjc.6605359
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605359
Keywords
This article is cited by
-
Risk factors for the postoperative recurrence of ulcerative colitis-associated colorectal cancer
International Journal of Colorectal Disease (2023)
-
Clinical features and oncological outcomes of intestinal cancers associated with ulcerative colitis and Crohn’s disease
Journal of Gastroenterology (2023)
-
Does Surveillance Increase Survival? Benefits of Periodic Colonoscopy in Patients with Ulcerative Colitis and Colorectal Cancer
Digestive Diseases and Sciences (2022)
-
State-of-the-art surgery for Crohn’s disease: Part II—colonic Crohn’s disease and associated neoplasms
Langenbeck's Archives of Surgery (2022)
-
Colitis ulcerosa
coloproctology (2021)