Primary care management of patients after weight loss surgery
BMJ 2016; 352 doi: https://doi.org/10.1136/bmj.i945 (Published 10 March 2016) Cite this as: BMJ 2016;352:i945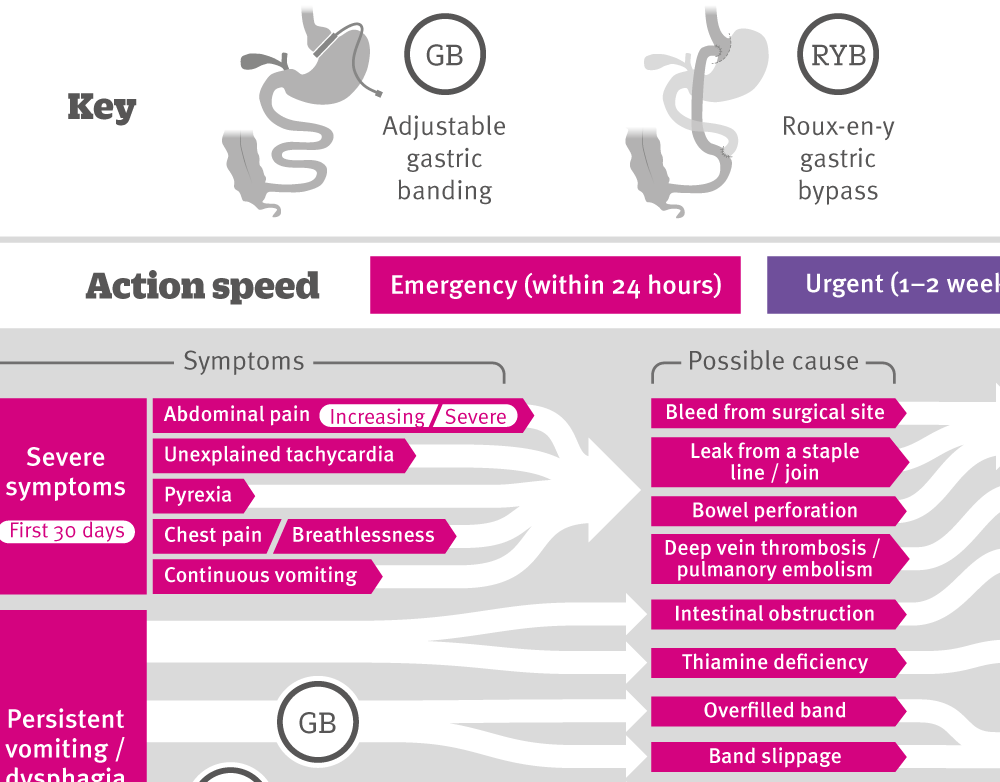
[Infographic] Assessing and referring complications following bariatric surgery
Explaining symptoms that warrant referral to bariatric and/or surgical teams, including possible causes, referral speed and recommended actions.

Chinese translation
该文章的中文翻译
- Michael Moore, professor of primary care research1,
- James Hopkins, senior bariatric fellow and honorary research fellow2 3,
- Patrick Wainwright, specialist registrar in chemical pathology and metabolic medicine4
- 1Primary Care and Population Sciences, Faculty of Medicine, University of Southampton, Southampton, UK
- 2Musgrove Park Hospital, Taunton, UK
- 3University of Bristol, Bristol, UK
- 4Clinical Biochemistry, University Hospital Southampton, Southampton, SO16 6YD, UK
- Correspondence to: M Moore mvm198{at}soton.ac.uk
What you need to know
In the first 30 days after bariatric surgery, symptoms such as increasing or severe abdominal pain, unexplained tachycardia, pyrexia, chest pain or breathlessness, or continuous vomiting warrant emergency referral
Continue long term monitoring of cardiovascular risk and comorbidities associated with obesity, such as type 2 diabetes; reduce treatment for these as appropriate
All patients need lifelong supplementation with vitamin and mineral supplements to prevent serious nutritional complications
Bariatric surgery is the most effective treatment for sustained weight loss in people with complex obesity,1 2 and reports from large UK and international registries highlight its overall safety.3 4 The overall mortality of 0.07% and composite complication rate of less than 4% for gastric bypass are similar to those for laparoscopic cholecystectomy.4 After surgery, short hospital stays are the norm (median one day for gastric band and two days for a sleeve gastrectomy or gastric bypass).2 General practitioners thus need to recognise early, as well as late, postoperative complications, monitor long term nutrition, and provide support. General practitioners may also need to assess patients who have had bariatric surgery abroad (sometimes with non-standard procedures), without any follow-up planned. Useful resources for patients include BOSPA (http://www.bospauk.org) and WLSinfo (http://www.wlsinfo.org.uk).
The operations
Box 1 describes the three most common procedures performed in the United Kingdom. More than 95% are done laparoscopically.3 5
Box 1: Most common bariatric surgery procedures in UK (fig 1⇓)
Laparoscopic adjustable gastric banding
An adjustable band is placed around the top of the stomach, forming a small gastric pouch above it. The band is adjusted by injecting saline into a port positioned under the skin to achieve the sensation of fullness after a small amount of food.
Roux-en-Y gastric bypass
The most common operation for weight loss in the UK NHS (60%), involving creation of a small gastric pouch by stapling. A classical Roux-en-Y reconstruction is then fashioned with a biliary limb carrying bile, pancreatic, and gastric secretions and an alimentary limb (connected to the new pouch) joined into a common channel for ongoing digestion.
Laparoscopic sleeve gastrectomy
Involves excising most (85%) of the stomach by stapling along a tube placed inside the stomach along the lesser curvature to create a narrow tube of stomach.
Fig 1 A: Gastric band surgery showing small “virtual” pouch of stomach below gastro-oesophageal junction and (inset) gastro-gastro tunnelling sutures. B: Gastric bypass showing short vertical lesser curve based gastric pouch with Roux-en-Y jejuno-jejunostomy reconstruction. C: Sleeve gastrectomy. (Images reproduced from Griffin SM, Raimes SA, Shenfine J. Oesophagogastric surgery. 5th ed. Saunders Elsevier, 2013)
What are the postoperative complications?
The infographic summarises the complications that can follow bariatric surgery and describes their causes and assessment.3 6 7 8 9 10 11 13
How to manage obesity related comorbidities after surgery
Patients are usually followed up every two to three months for the first two years by the bariatric multidisciplinary team, then yearly by general practitioners in a shared care model.12 Continue monitoring cardiovascular risk and comorbidities associated with obesity, being mindful of possible de-escalation of their treatment13:
Type 2 diabetes—No clear consensus exists on long term management of such patients, but Endocrine Society guidelines recommend measuring glycated haemoglobin (HbA1c) at least annually.11 Up to 65% of patients with type 2 diabetes may be in glycaemic remission two years after surgery and may be able to stop their antidiabetes drugs.3 14 Longer term follow-up data suggest that up to one third of patients who initially experience glycaemic remission will go on to redevelop diabetes within five years of gastric bypass.15
Hypertension—At each blood pressure review, evaluate the need for antihypertensive drugs. The effect of weight loss is variable and often transient, although many patients can reduce or stop antihypertensive drugs.16
Dyslipidaemia—Bariatric surgery is known to reduce total cholesterol, low density lipoprotein cholesterol, and triglycerides while increasing high density lipoprotein cholesterol.17 In the light of other comorbidities, however, patients may remain at increased cardiovascular risk. Consider statin treatment in line with recent recommendations from the National Institute for Health and Care Excellence.18
What are the postoperative nutritional requirements and how should they be monitored?
High quality evidence to guide clinicians is lacking here, although the British Obesity and Metabolic Surgery Society (BOMSS) has recently published recommendations based on observational data (table 1⇓).19 20 These recommend that all patients who have had bariatric surgery should take a complete multivitamin and mineral supplement, in addition to further supplementation in most cases. Patients who have had bariatric surgery will often need much higher than standard recommended doses of supplementation to become replete. Patients need careful biochemical monitoring, depending on the type of procedure. Table 2⇓ outlines the BOMSS recommendations.20
What about bone health?
Compared with dietary weight loss, bariatric surgery procedures such as Roux-en-Y gastric bypass (which bypasses the main sites of calcium absorption) may lead to calcium deficiency, secondary hyperparathyroidism, increased vitamin D activation, and increased calcium resorption from bone resulting in a disproportionate amount of bone loss.21 The clinical significance of this state is unclear, and a retrospective population study of more than 2000 bariatric surgery patients did not find a statistically significantly increased risk of fracture in the two years after surgery.22 Gastric bypass is generally associated with less bone loss than Roux-en-Y gastric bypass.
Supplementation—Patients should take calcium and vitamin D supplementation according to their preoperative status (table 1⇑), although some may need a higher maintenance dose of vitamin D, occasionally up to 4000 IU daily.11
Monitoring—Table 2⇑ outlines blood monitoring requirements for calcium and vitamin D. Little evidence is available, and thus no firm consensus exists, on the role of dual energy x ray absorptiometry (DEXA) for routine monitoring. Some guidelines suggest considering DEXA scans at baseline and two years after surgery in patients who have had Roux-en-Y gastric bypass,16 whereas others advise yearly DEXA until bone density is stable.11
Osteoporosis treatment—If DEXA scanning identifies osteoporosis, evaluate calcium and vitamin D status and treat any abnormalities before considering bisphosphonate treatment. Offer intravenous bisphosphonates such as zoledronic acid, owing to concerns about oral absorption and the potential for anastomotic ulceration.
Are there precautions regarding pregnancy?
Pregnancy is considered safe after bariatric surgery, as most maternal (pre-eclampsia, gestational diabetes) and fetal complications (macrosomia) of obesity are reduced after weight loss surgery.23 However, most guidelines advise avoiding pregnancy preoperatively and for 18 months after surgery, on the basis of low quality evidence suggesting a risk of fetal growth retardation from nutritional deficiencies in rapid weight loss. Offer non-oral contraception for sleeve and bypass patients16; any methods of contraception are suitable for band patients. Pregnancy should trigger a review by the bariatric multidisciplinary team, as routine band deflation or additional nutritional supplementation may be needed.
What if the patient regains weight?
Patients often regain 20-25% of their lost weight over a 10 year period after surgery.24 Greater regain may cause obesity related comorbidities to re-emerge.
Figure 2⇓ outlines possible reasons for weight regain based on a systematic review,25 with our suggested questions to open up discussion of these reasons with the patient. Patient related factors are more common; however, as with any prosthetic or anatomical modification, the procedure can fatigue.
Fig 2 Patient related and surgical factors in weight regain,25 and questions that may help the practitioner to recognise the underlying cause
The most important aspect in managing weight regain after bariatric surgery is continued engagement with healthcare services. Early assessment by a bariatric dietitian may also identify surgical complications (commonly suggested by new or increased heartburn or reflux) requiring re-referral to the surgical team.
Search strategy
We based this predominantly on current guidelines and systematic reviews
Additional references were drawn from our personal datasets
How patients were involved
We discussed the article with a patient representative from two bariatric patient groups, BOSPA and WLSinfo, who reviewed the article as it was being written. We incorporated their suggestions on the commonly unclear nature of symptoms that patients experience in the section on complications. The contribution of one author (JH) was also informed by a survey of more than 100 patients on aspects important to them, conducted by Karen Coulman (University of Bristol for an NIHR funded doctoral research fellowship), in which he collaborated as part the ByBand Trial.26
Footnotes
James Byrne and Sean Woodcock, consultant bariatric surgeons and members of the BOMSS Council, reviewed this paper, as did Ken Clare, chairman of WLSinfo (a patient led charity providing web based support and information) and retired bariatric specialist nurse. We are grateful for advice and comments from Christopher Byrne, professor of diabetes, University of Southampton.
Contributors: All authors made substantial contributions to the text and were involved in drafting and revision of the work and in final approval. All authors accept responsibility for the accuracy and integrity of the work. MM is the guarantor.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: none.
Provenance and peer review: Commissioned; externally peer reviewed.


